INTRODUCTION: Production of erythrocytes in the marrow occurs at the staggering rate of more than 2 million cells per second. For this production to occur, a number of raw materials must be present in adequate amounts. These include the same nutrients that are essential to the production and maintenance of any cell, such as glucose, lipids, and amino acids. However, erythrocyte production also requires several trace elements:
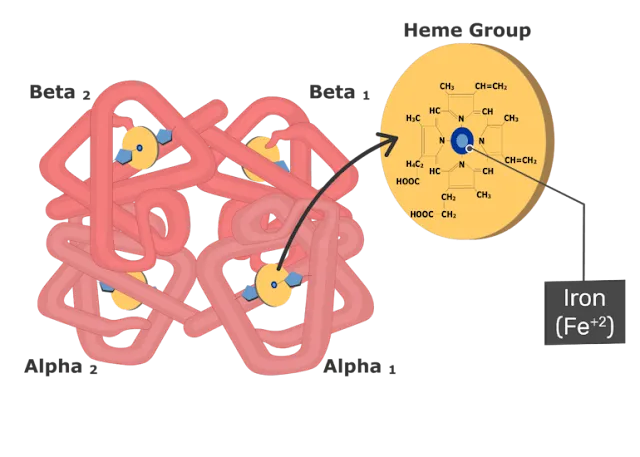
1) Iron: Each heme group in a hemoglobin molecule contains an ion of the trace mineral iron. On average, less than 20 percent of the iron we consume is absorbed. Heme iron, from animal foods such as meat, poultry, and fish, is absorbed more efficiently than non-heme iron from plant foods. Upon absorption, iron becomes part of the body’s total iron pool. The bone marrow, liver, and spleen can store iron in the protein compounds ferritin and hemosiderin. Ferroportin transports the iron across the intestinal cell plasma membranes and from its storage sites into tissue fluid where it enters the blood. When EPO stimulates the production of erythrocytes, iron is released from storage, bound to transferrin, and carried to the red marrow where it attaches to erythrocyte precursors.
2) Copper: A trace mineral, copper is a component of two plasma proteins, hephaestin and ceruloplasmin. Without these, hemoglobin could not be adequately produced. Located in intestinal villi, hephaestin enables iron to be absorbed by intestinal cells. Ceruloplasmin transports copper. Both enable the oxidation of iron from Fe2+ to Fe3+, a form in which it can be bound to its transport protein, transferrin, for transport to body cells. In a state of copper deficiency, the transport of iron for heme synthesis decreases, and iron can accumulate in tissues, where it can eventually lead to organ damage.
3) Zinc: The trace mineral zinc functions as a co-enzyme that facilitates the synthesis of the heme portion of hemoglobin.
4) B vitamins: The B vitamins folate and vitamin B12 function as co-enzymes that facilitate DNA synthesis. Thus, both are critical for the synthesis of new cells, including erythrocytes. Erythrocytes live up to 120 days in the circulation, after which the worn-out cells are removed by a type of myeloid phagocytic cell called a macrophage, located primarily within the bone marrow, liver, and spleen. The components of the degraded erythrocytes’ hemoglobin are further processed as follows: 1) Globin, the protein portion of hemoglobin, is broken down into amino acids, which can be sent back to the bone marrow to be used in the production of new erythrocytes. Hemoglobin that is not phagocytized is broken down in the circulation, releasing alpha and beta chains that are removed from circulation by the kidneys. 2) The iron contained in the heme portion of hemoglobin may be stored in the liver or spleen, primarily in the form of ferritin or hemosiderin, or carried through the bloodstream by transferrin to the red bone marrow for recycling into new erythrocytes. 3) The non-iron portion of heme is degraded into the waste product biliverdin, a green pigment, and then into another waste product, bilirubin, a yellow pigment. Bilirubin binds to albumin and travels in the blood to the liver, which uses it in the manufacture of bile, a compound released into the intestines to help emulsify dietary fats.
In the large intestine, bacteria breaks the bilirubin apart from the bile and converts it to urobilinogen and then into stercobilin. It is then eliminated from the body in the feces. Broad-spectrum antibiotics typically eliminate these bacteria as well and may alter the color of feces. The kidneys also remove any circulating bilirubin and other related metabolic byproducts such as urobilins and secrete them into the urine.
The breakdown pigments formed from the destruction of hemoglobin can be seen in a variety of situations. At the site of an injury, biliverdin from damaged RBCs produces some of the dramatic colors associated with bruising. With a failing liver, bilirubin cannot be removed effectively from circulation and causes the body to assume a yellowish tinge associated with jaundice. Stercobilins within the feces produce the typical brown color associated with this waste. And the yellow of urine is associated with the urobilins.
RELATED;













No comments:
Post a Comment