HUMAN ANATOMY: the discipline of human anatomy deals with the organization of the human body and the way body organs are arranged in relation to each other. It is only when we know very well this type of organisation that we can be able to allocate abnormalities and their possible causes when it comes to disease states. In our discussion here, we are going to be looking at some of the most visible and immediate human body organs and the way they are related to each other. You may also want to read about the following disciplines; Human physiology,
THE WORLD IS CHANGING NOWADAYS ESPECIALLY WHEN IT COMES TO EDUCATION. DURING THIS PERIOD AND POST COVID 19 PANDEMIC, A MODERN MEDICAL SCHOLAR WILL NEED TO BE UPDATED WITH THE LATEST ICT SKILLS TO MEET THE CHALLENGES OF THE PAST. THIS SITE WAS CREATED AT THE BEGINNING OF COVID 19 LOCKDOWN WITH THE AIM TO PROVIDE MEDICAL STUDENTS WITH SELF STUDY NOTES IN MEDICINE, PHARMACOLOGY, RESEARCH METHODS, MICROBIOLOGY, PATHOPHYSIOLOGY AND BIOCHEMISTRY.
October 18, 2023
HUMAN ANATOMY
 Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
May 13, 2023
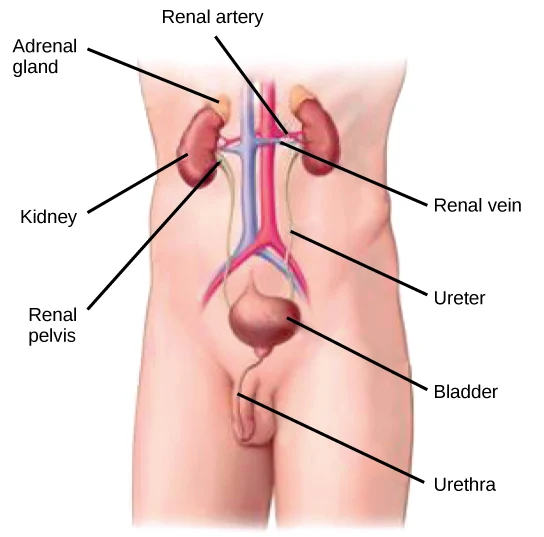
THE HUMAN KIDNEYS
INTRODUCTION: The two kidneys are located in the upper abdominal cavity on either side of the vertebral column, behind the peritoneum. The upper portions of the kidneys rest on the lower surface of the diaphragm and are enclosed and protected by the lower rib cage. The kidneys are embedded in adipose tissue that acts as a cushion and is in turn covered by a fibrous connective tissue membrane called the renal fascia, which helps hold the kidneys in place.
BASIC ANATOMY OF THE KIDNEY: Each kidney has an indentation called the hilus on its medial side. At the hilus, the renal artery enters the kidney, and the renal vein and ureter emerge. The renal artery is a branch of the abdominal aorta, and the renal vein returns blood to the inferior vena cava. The ureter carries urine from the kidney to the urinary bladder.
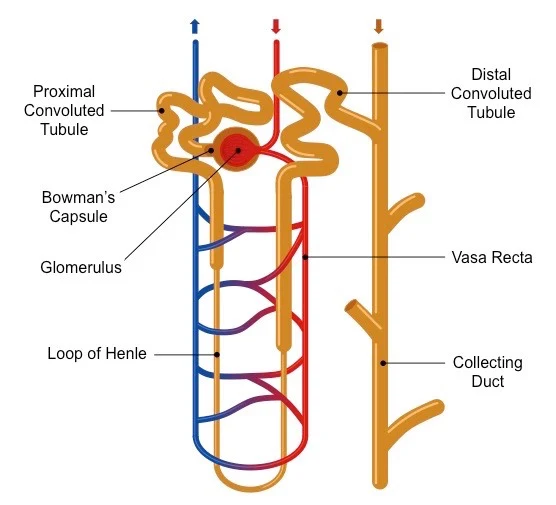
INTERNAL STRUCTURE OF THE KIDNEY: In a coronal or frontal section of the kidney, three areas can be distinguished. The lateral and middle areas are tissue layers, and the medial area at the hilus is a cavity. The outer tissue layer is called the renal cortex; it is made of renal corpuscles and convoluted tubules. These are parts of the nephron and are described in details in our next discussion. The inner tissue layer is the renal medulla, which is made of loops of Henle and collecting tubules which are also, parts of the nephron. The renal medulla consists of wedge-shaped pieces called renal pyramids. The tip of each pyramid is its apex or papilla. The third area is the renal pelvis, and this is not a layer of tissues, but rather a cavity formed by the expansion of the ureter within the kidney at the hilus. Funnel shaped extensions of the renal pelvis, called calyces or in singular: calyx, enclose the papillae of the renal pyramids. Urine flows from the renal pyramids into the calyces, then to the renal pelvis and out into the ureter.
THE NEPHRON: The nephron is the structural and functional unit of the kidney. Each kidney contains approximately 1 million nephrons. It is in the nephrons, with their associated blood vessels, that urine is formed. Each nephron has two major portions: a renal corpuscle and a renal tubule. Each of these major parts has further subdivisions, and we shall discuss more about them later.
RELATED;
3. ALDOSTERONE
 Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
May 12, 2023
THE HUMAN SPLEEN
INTRODUCTION: The spleen is located in the upper left quadrant of the abdominal cavity, just below the diaphragm, behind the stomach. The lower rib cage protects the spleen from physical trauma and it is one of the organs in the human body that plays various roles in immunity as discussed in our previous articles. In the fetus, the spleen produces red blood cells, a function assumed by the red bone marrow after birth. After birth the spleen is very much like a large lymph node, except that its functions affect the blood that flows through it rather than lymph.
FUNCTIONS OF THE SPLEEN: The functions of the spleen after birth are:
1. Contains plasma cells that produce antibodies to foreign antigens.
2. Contains fixed macrophages (RE cells) that phagocytize pathogens or other foreign material in the blood. The macrophages of the spleen also phagocytize old red blood cells and form bilirubin and by way of portal circulation, the bilirubin is sent to the liver for excretion in bile.
3. Stores platelets and destroys them when they are no longer useful.
SIGNIFICANCE OF THE SPLEEN: The spleen is not considered a vital organ, because other organs compensate for its functions if the spleen must be removed, in a surgical procedure known as spleenectomy. The liver and red bone marrow will remove old red blood cells and platelets from circulation. The many lymph nodes and nodules plus the liver, will phagocytize pathogens and have lymphocytes to be activated and plasma cells to produce antibodies. It should however be noted that, a person without a spleen is somewhat more susceptible to certain bacterial infections such as pneumonia and meningitis.
RELATED;
3. THE LIVER
4. METABOLIC PROFILE OF ORGANS
5. IMMUNITY
 Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
May 05, 2023
STEM CELLS
INTRODUCTION: Stem cells are characterized by their ability of possessing self-renewal capability and capacity to generate differentiated cell lineages. These cells in short terms are broad in perspective that later in their life span, can give rise to different cell types.
PROPERTIES OF STEM CELLS: There are different cellular properties that would otherwise be absent in other cell types and let us briefly look at them.
1. Self-renewal capacity and capacity to generate differentiated cell lineages. Here, a stem cell will be able to regain it’s ability to carry out cellular activities following damage or destruction, and then be able to divide and even produce other cell types.
2. Asymmetric replication: This is characterized by division of stem cell into two cells: One daughter cell which gives rise to mature cells, and then the other cell remains as undifferentiated stem cell which retains the self-renewal capacity.
TYPES OF STEM CELLS: Stem cells are of different types and located in different parts of the body.
1. Embryonic stem cells: During development of embryo, the blastocysts contain undifferentiated pluripotent stem cells, which are called as embryonic stem cells or ES cells. These cells can form cells of all three germ cell layers. Their normal function is to give rise to all cells of the human body.
2. Adult or sometimes known as somatic stem cells: Adult stem cells are less undifferentiated than ES cells found in adults. They are found among differentiated cells within a tissue. They have more limited capacity to generate different cell types than ES cells. They usually differentiate into particular tissue. Their normal function is tissue homeostasis.
3. Induced pluripotent stem cells (iPS cells): This is achieved by transferring the nucleus of adult cells to an enucleated oocyte. These are used for therapeutic cloning in the treatment of human diseases.
SITES OF STEM CELLS
1. Bone marrow: This contains two types of stem cells; The Hematopoietic stem cells (HSCs), and these can generate all of the blood cell lineages, and are used for the treatment of hematologic diseases. They can also be collected directly from the bone marrow, from umbilical cord blood, and from the peripheral blood. The other type are the Marrow stromal cells (MSCs): They can generate chondrocytes, osteoblasts, adipocytes, myoblasts, and endothelial cell precursors depending on the tissue to which they migrate.
2. Intestinal epithelium: Stem cells may be located immediately above Paneth cells in the small intestine or at the base of the crypt in the colon.
3. Liver: The liver contains stem cell in the canals of Hering, which are capable of differentiating into hepatocytes and biliary cells.
4. Cornea: Located in the limbus region between the conjunctiva and the cornea.
5. Skin: Located in the bulge area of the hair follicle, in the sebaceous glands, and in the lower layer of the epidermis.
RELATED;
1. FORMED ELEMENTS FROM STEM CELLS
 Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
May 01, 2023
ADRENAL GLANDS
INTRODUCTION: The two adrenal glands are located one on top of each kidney, which gives them their other name of suprarenal glands. Each adrenal gland consists of two parts: an inner adrenal medulla and an outer adrenal cortex. The hormones produced by each part have very different functions.
ADRENAL MEDULLA: The cells of the adrenal medulla secrete epinephrine and norepinephrine, which collectively are called catecholamines and are sympathomimetic. The section of both hormones is stimulated by sympathetic impulses from the hypothalamus, and their functions duplicate and prolong those of the sympathetic division of the autonomic nervous system.
EPINEPHRINE AND NOREPINEPHRINE: Epinephrine also known as Adrenalin and norepinephrine also known as noradrenalin, are both secreted in stress situations and help prepare the body for the so called fight or flight response. Norepinephrine is secreted in small amounts, and its most significant function is to cause vasoconstriction in the skin, viscera, and skeletal muscles throughout the body, which raises blood pressure.
The other counterpart epinephrine, secreted in larger amounts, increases the heart rate and force of contraction and stimulates vasoconstriction in skin and viscera and vasodilation in skeletal muscles. It also dilates the bronchioles, decreases peristalsis, stimulates the liver to change glycogen to glucose, increases the use of fats for energy, and increases the rate of cell respiration. Epinephrine in this sense, is more effective than sympathetic stimulation, however, because the hormone increases energy production and cardiac output to a greater extent.
ADRENAL CORTEX: The adrenal cortex secretes three types of steroid hormones;
1. Mineralocorticoids,
2. Glucocorticoids, and
3. Sex hormones.
The sex hormones which for females are the estrogens and for the males are the androgens baring some similarity to testosterone, are produced in very small amounts contribute to rapid body growth during early puberty. They may also be important in supplying estrogen to women after menopause and to men throughout life and are discussed in our previous discussions as in the links below.
RELATED;
1. EPINEPHRINE
2. THE NEUROTRANSMITTER SYSTEMS
3. DOPAMINE
 Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
April 30, 2023
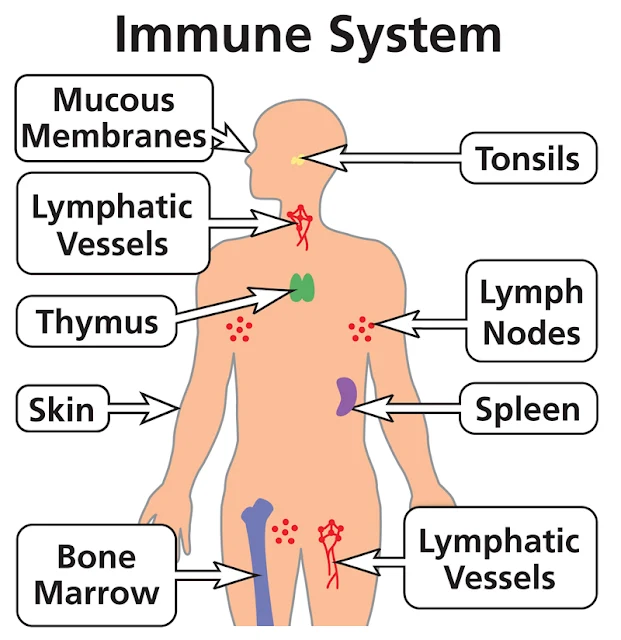
ORGANS OF THE IMMUNE SYSTEM
INTRODUCTION: Several tissues and organs play roles in host defenses and are functionally classified as the immune system. In the human body, the primary immune parts are the lymphoid organs; the thymus and the bone marrow. All cells of the immune system are originally derived from bone marrow and that cellular lineage is known as the Pluripotent stem cells.
IMMUNE CELLS FROM THE BONE MALLOW: Pluripotent stem cells differentiate into lymphocyte, granulocyte, monocyte, erythrocyte, and megakaryocyte populations. Deficiency or dysfunction of the pluripotent stem cell or the various cell lines developing from it can result in immune deficiency disorders of varying expression and severity.
THYMUS GLAND AND IT’S ROLE IN IMMUNITY: The thymus, derived from the third and fourth embryonic pharyngeal pouches, functions to produce T lymphocytes and is the site of initial T lymphocyte differentiation. Developing T cells in the thymic cortex are first positively selected for their ability to recognize self-peptides which are, major histocompatibility complex (MHC). In subsequent negative selection, T cells that avidly recognize self-peptides are destroyed, thus removing deleterious self-reactive clones. The thymus also regulates immune function by secreting multiple bioactive substances that promote T-lymphocyte differentiation and are essential for T-lymphocyte–mediated immunity.
OTHER LYMPHOID ORGANS IN THE HUMAN BODY: In mammals, the lymph nodes, spleen, and gut-associated lymphoid tissue are secondary lymphoid organs connected by blood and lymphatic vessels. Lymph nodes are strategically dispersed throughout the vasculature and are the principal organs of the immune system that deliver and localize antigen, promoting adaptive immunity through cell–cell interaction and lymphocyte activation.
LYMPH NODE AND THEIR ROLE IN IMMUNITY: Lymph nodes have a framework of reticular cells and fibers that are arranged into a cortex and medulla. B lymphocytes, the precursors of antibody-producing cells, or plasma cells, are found in the cortex, as well as in the medulla. T lymphocytes are found chiefly in the medullary and paracortical areas of the lymph node.
THE SPLEEN AND IT’S ROLE IN IMMUNITY: The spleen filters and processes antigens from the blood and is functionally and structurally divided into B-lymphocyte and T-lymphocyte areas, similar to those of the lymph nodes. The spleen also removes damaged blood cells and immune complexes, including antibody-coated microbes. Loss of the spleen, through traumatic causes or therapeutic splenectomy, increases host susceptibility to encapsulated bacteria, which are normally cleared through opsonization and phagocytosis in splenic tissue.
THE GASTROINTESTINAL TRACT AND IT’S ROLE IN IMMUNITY: Gut-associated lymphoid tissue, adjacent to the mucosal epithelium, includes the tonsils, the Peyer patches of the small intestine, and the appendix, all of which facilitate immune responses to the multitude of ingested antigens and commensal microbes. Like the lymph nodes and spleen, these tissues exhibit separation into B-lymphocyte–dependent and T-lymphocyte–dependent areas. Mucosal immune responses tend to generate antigen-specific IgA, and, with some orally administered antigens, T-cell anergy or tolerance may occur rather than immune stimulation. Increasingly, the commensal microbiome of the gastrointestinal tract has been recognized to shape both local and systemic innate and adaptive immune responses, influencing both health and disease for example the case of allergy or autoimmunity.
RELATED;
1. LINEAGES OF STEM CELLS FROM THE BORN MARROW
2. THE MAJOR HISTOCOMPATIBILITY COMPLEX
5. ALLERGY
6. AUTOIMMUNITY
 Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
December 11, 2022
LIVER
INTRODUCTION: The liver consists of two large lobes, right and left, and fills the upper right and center of the abdominal cavity, just below the diaphragm. The structural unit of the liver is the liver lobule, a roughly hexagonal column of liver cells (hepatocytes). Between adjacent lobules are branches of the hepatic artery and portal vein. The capillaries of a lobule are sinusoids, large and very permeable vessels between the rows of liver cells. The sinusoids receive blood from both the hepatic artery and portal vein, and it is with this mixture of blood that the liver cells carry out their functions.
BLOOD SUPPLY OF THE LIVER: The hepatic artery brings oxygenated blood, and the portal vein brings blood from the digestive organs and spleen. Each lobule has a central vein. The central veins of all the lobules unite to form the hepatic veins, which take blood out of the liver to the inferior vena cava. The cells of the liver have many functions, but their only digestive function is the production of bile.
ROLE OF BILE IN DIGESTION: Bile enters the small bile ducts, called bile canaliculi, on the liver cells, which unite to form larger ducts and finally merge to form the hepatic duct, which takes bile out of the liver. The hepatic duct unites with the cystic duct of the gallbladder to form the common bile duct, which takes bile to the duodenum. Bile is mostly water and has an excretory function in that it carries bilirubin and excess cholesterol to the intestines for elimination in feces. The digestive function of bile is accomplished by bile salts, which emulsify fats in the small intestine. Emulsification means that large fat globules are broken into smaller globules. This is mechanical, not chemical, digestion; the fat is still fat but now has more surface area to facilitate chemical digestion. Production of bile is stimulated by the hormone secretin, which is produced by the duodenum when food enters the small intestine.
RELATED;
3. HEPATITIS
 Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
September 29, 2022
THE ACTION POTENTIAL
INTRODUCTION: The functions of the nervous system sensation, integration, and response depend on the functions of the neurons underlying these pathways. To understand how neurons are able to communicate, it is necessary to describe the role of an excitable membrane in generating these signals. The basis of this communication is the action potential, which demonstrates how changes in the membrane can constitute a signal. Looking at the way these signals work in more variable circumstances involves a look at graded potentials.
ELECTRICALLY ACTIVE CELL MEMBRANES: Most cells in the body make use of charged particles, ions, to build up a charge across the cell membrane. Previously, this was shown to be a part of how muscle cells work. For skeletal muscles to contract, based on excitation–contraction coupling, requires input from a neuron. Both of the cells make use of the cell membrane to regulate ion movement between the extracellular fluid and cytosol. The cell membrane is primarily responsible for regulating what can cross the membrane and what stays on only one side. The cell membrane is a phospholipid bilayer, so only substances that can pass directly through the hydrophobic core can diffuse through unaided. Solubility of compounds
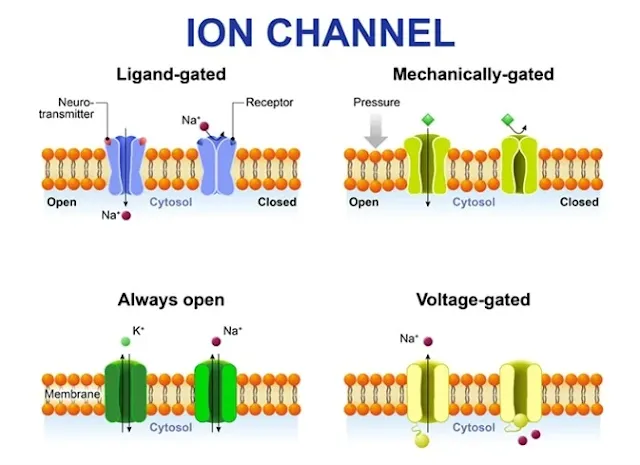
Charged particles, which are hydrophilic by definition, cannot pass through the cell membrane without assistance. Transmembrane proteins, specifically channel proteins, make this possible. Several channels, as well as specialized energy dependent ion-pumps, are necessary to generate a transmembrane potential and to generate an action potential.
THE SODIUM/POTASSIUM PUMP: Of special interest is the carrier protein referred to as the sodium/potassium pump that moves sodium ions (Na+) out of a cell and potassium ions (K+) into a cell, thus regulating ion concentration on both sides of the cell membrane. The sodium/potassium pump requires energy in the form of adenosine triphosphate (ATP), so it is also referred to as an ATPase. The concentration of Na+ is higher outside the cell than inside, and the concentration of K+ is higher inside the cell is higher than outside. That means that this pump is moving the ions against the concentration gradients for sodium and potassium, which is why it requires energy. In fact, the pump basically maintains those concentration gradients.
ION CHANNELS: Ion channels are pores that allow specific charged particles to cross the membrane in response to an existing concentration gradient. Proteins are capable of spanning the cell membrane, including its hydrophobic core, and can interact with the charge of ions because of the varied properties of amino acids found within specific domains or regions of the protein channel. Hydrophobic amino acids are found in the domains that are apposed to the hydrocarbon tails of the phospholipids. Hydrophilic amino acids are exposed to the fluid environments of the extracellular fluid and cytosol. Additionally, the ions will interact with the hydrophilic amino acids, which will be selective for the charge of the ion. Channels for cations (positive ions) will have negatively charged side chains in the pore. Channels for anions (negative ions) will have positively charged side chains in the pore. This is called electrochemical exclusion, meaning that the channel pore is charge-specific.
RELATED;
1. PROPAGATION OF A NERVE IMPULSE
2. DIVISIONS OF THE NERVOUS SYSTEM
3. THE SYNAPSE
 Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
June 08, 2022
THE HUMAN SKIN
 Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
March 23, 2022
CHAMBERS AND CIRCULATION THROUGH THE HEART
Introduction: The human heart consists of four chambers: The left side and the right side each have one atrium and one ventricle. Each of the upper chambers, the right atrium and the left atrium, acts as a receiving chamber and contracts to push blood into the lower chambers, the right ventricle and the left ventricle. The ventricles serve as the primary pumping chambers of the heart, propelling blood to the lungs or to the rest of the body. There are two distinct but linked circuits in the human circulation called the pulmonary and systemic circuits. Although both circuits transport blood and everything it carries, we can initially view the circuits from the point of view of gases. The pulmonary circuit transports blood to and from the lungs, where it picks up oxygen and delivers carbon dioxide for exhalation.
 Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
March 21, 2022
THE HUMAN RED BLOOD CELLS
INTRODUCTION: The erythrocyte, commonly known as a red blood cell (or RBC), is by far the most common formed element: A single drop of blood contains millions of erythrocytes and just thousands of leukocytes. Specifically, males have about 5.4 million erythrocytes per microliter (µL) of blood, and females have approximately 4.8 million per µL. In fact, erythrocytes are estimated to make up about 25 percent of the total cells in the body. The primary functions of erythrocytes are to pick up inhaled oxygen from the lungs and transport it to the body’s tissues, and to pick up some carbon dioxide waste at the tissues and transport it to the lungs for exhalation. Erythrocytes remain within the vascular network. Although leukocytes typically leave the blood vessels to perform their defensive functions, movement of erythrocytes from the blood vessels is abnormal.
Shape and Structure of Erythrocytes: As an erythrocyte matures in the red bone marrow, it extrudes its nucleus and most of its other organelles. During the first day or two that it is in the circulation, an immature erythrocyte, known as a reticulocyte, will still typically contain remnants of organelles. Reticulocytes should comprise approximately 1–2 percent of the erythrocyte count and provide a rough estimate of the rate of RBC production, with abnormally low or high rates indicating deviations in the production of these cells. These remnants, primarily of networks (reticulum) of ribosomes, are quickly shed, however, and mature, circulating erythrocytes have few internal cellular structural components. Lacking mitochondria, for example, they rely on anaerobic respiration. This means that they do not utilize any of the oxygen they are transporting, so they can deliver it all to the tissues. They also lack endoplasmic reticula and do not synthesize proteins. Erythrocytes do, however, contain some structural proteins that help the blood cells maintain their unique structure and enable them to change their shape to squeeze through capillaries. This includes the protein spectrin, a cytoskeletal protein element.
Shape of erythrocytes: Erythrocytes are biconcave disks; that is, they are plump at their periphery and very thin in the center. Since they lack most organelles, there is more interior space for the presence of the hemoglobin molecules that, as you will see shortly, transport gases. The biconcave shape also provides a greater surface area across which gas exchange can occur, relative to its volume; a sphere of a similar diameter would have a lower surface area-to-volume ratio. In the capillaries, the oxygen carried by the erythrocytes can diffuse into the plasma and then through the capillary walls to reach the cells, whereas some of the carbon dioxide produced by the cells as a waste product diffuses into the capillaries to be picked up by the erythrocytes. Capillary beds are extremely narrow, slowing the passage of the erythrocytes and providing an extended opportunity for gas exchange to occur. However, the space within capillaries can be so minute that, despite their own small size, erythrocytes may have to fold in on themselves if they are to make their way through. Fortunately, their structural proteins like spectrin are flexible, allowing them to bend over themselves to a surprising degree, then spring back again when they enter a wider vessel. In wider vessels, erythrocytes may stack up much like a roll of coins, forming a rouleaux, from the French word for “roll.”
RELATED;
3. HEMOGLOBIN
 Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
February 18, 2022
LEUKOCYTES
Characteristics of Leukocytes: Although leukocytes and erythrocytes both originate from hematopoietic stem cells in the bone marrow, they are very different from each other in many significant ways. For instance, leukocytes are far less numerous than erythrocytes: Typically there are only 5000 to 10,000 per µL. Bloodand its components
 Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
January 14, 2022
BODY ORGANS
 Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
December 20, 2021
MAJOR HISTOCOMPATIBILITY COMPLEX (MHC)
INTRODUCTION: By virtue of genetic make-up, every individual has unique antigens on the cell surfaces. Some of these are called as histocompatibility (histo: tissue) antigens. These are responsible for determining whether one tissue is compatible with another. In human beings these antigens are called as human leukocyte antigens (HLA). Expression of histocompatibility antigens is controlled by genes or groups of genes (loci) located close together (linked) on the same chromosomal strand. This segment of chromosome is called major histocompatibility complex, or MHC.
 Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
November 10, 2021
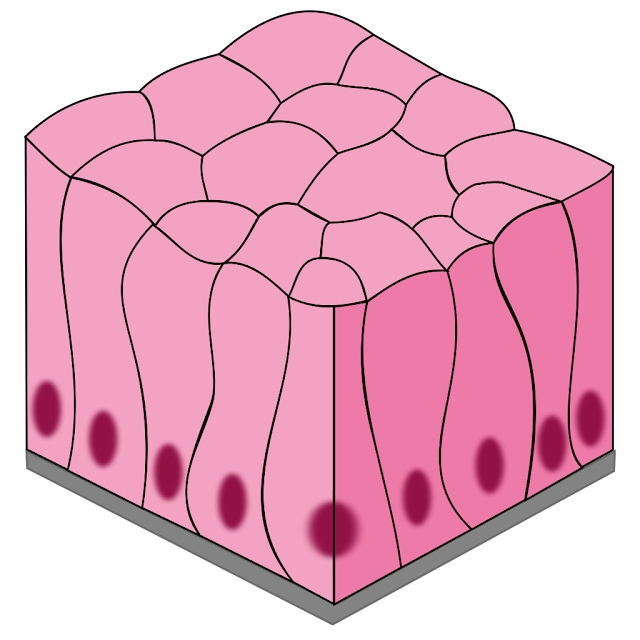
TISSUES
EPITHELIAL TISSUE: Epithelial tissues are found on surfaces as either coverings for the outer surfaces, or linings for the inner surfaces. Because they have no capillaries of their own, epithelial tissues receive oxygen and nutrients from the blood supply of the connective tissue beneath them. Many epithelial tissues are capable of secretion and may be called glandular epithelium, or more simply, glands. Classification of the epithelial tissues is based on the type of cell of which the tissue is made, its characteristic shape, and the number of layers of cells. There are three distinctive shapes: squamous cells are flat, cuboidal cells are cube shaped, and columnar cells are tall and narrow. “Simple” is the term for a single layer of cells, and “stratified” means that many layers.
SIMPLE SQUAMOUS EPITHELIUM: Simple squamous epithelium is a single layer of flat cells. These cells are very thin and very smooth. The alveoli (air sacs) of the lungs are simple squamous epithelium. The thinness of the cells permits the diffusion of gases between the air and blood. Another location of this tissue is capillaries, the smallest blood vessels. Capillary walls are only one cell thick, which permits the exchange of gases, nutrients, and waste products between the blood and tissue fluid. The interior surface of capillaries is also very smooth. These cells continue as the lining of the arteries, veins, and heart; this is important because it prevents abnormal blood clotting within blood vessels.
STRATIFIED SQUAMOUS EPITHELIUM: Stratified squamous epithelium consists of many layers of mostly flat cells, although lower cells are rounded. Mitosis takes place in the lowest layer to continually produce new cells to replace those worn off the surface. This type of epithelium makes up the epidermis of the skin, where it is called keratinizing because the protein keratin is produced, and the surface cells are dead. Stratified squamous epithelium of the non-keratinizing type lines the oral cavity, the esophagus, and, in women, the vagina. In these locations the surface cells are living and make up the mucous membranes of these organs. In all of its body locations, this tissue is a barrier to microorganisms because the cells of which it is made are very close together.
TRANSITIONAL EPITHELIUM: Transitional epithelium is a type of stratified epithelium in which the surface cells change shape from round to squamous. The urinary bladder is lined with transitional epithelium. When the bladder is empty, the surface cells are rounded. As the bladder fills, these cells become flattened. Transitional epithelium enables the bladder to fill and stretch without tearing the lining.
SIMPLE CUBOIDAL EPITHELIUM: Simple cuboidal epithelium is a single layer of cube-shaped cells. This type of tissue makes up the functional units of the thyroid gland and salivary glands. These are examples of glandular epithelium; their function is secretion. In these glands the cuboidal cells are arranged in small spheres and secrete into the cavity formed by the sphere. In the thyroid gland, the cuboidal epithelium secretes the thyroid hormones; thyroxine is an example. In the salivary glands the cuboidal cells secrete saliva. Cuboidal epithelium also makes up portions of the kidney tubules. Here the cells have microvilli, and their function is the reabsorption of useful materials back to the blood.
SIMPLE COLUMNAR EPITHELIUM: Columnar cells are taller than they are wide and are specialized for secretion and absorption. The stomach lining is made of columnar epithelium that secretes gastric juice for digestion. The lining of the small intestine secretes digestive enzymes, but these cells also absorb the end products of digestion from the cavity of the intestine into the blood and lymph. To absorb efficiently, the columnar cells of the small intestine have microvilli, which you may recall are folds of the cell membrane on their free surfaces. These microscopic folds greatly increase the surface area for absorption. Yet another type of columnar cell is the goblet cell, which is a unicellular gland. Goblet cells secrete mucus and are found in the lining of the intestines and the lining of parts of the respiratory tract such as the trachea.
CILIATED EPITHELIUM: Ciliated epithelium consists of columnar cells that have cilia on their free surfaces. Ciliated epithelium lines the nasal cavities, larynx, trachea, and large bronchial tubes. The cilia sweep mucus, with trapped dust and bacteria from the inhaled air, toward the pharynx to be swallowed. Bacteria are then destroyed by the hydrochloric acid in the stomach. The air that reaches the lungs is almost entirely free of pathogens and particulate pollution. Another location of ciliated epithelium in women is the lining of the fallopian tubes. The cilia here sweep the ovum, which has no means of self-locomotion, toward the uterus.
RELATED;
 Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
Godfrey Kateregga as the author and administrator of this page, is a Ugandan youth male Graduate from Mbarara University of Science and Technology, Faculty of Medicine, Western Uganda. He is a medical scientist with over half a decade in instructing medical students and, interested in sharing medical information and medical informatics plus ICT, widely experienced in training Adults with special needs.
MOST FREQUENTLY READ
-
GOSPEL MUSIC DOWNLOADS: Music is part of the daily life and for some of us, working while listening to music is a daily routine. On this p...
-
ACTIONS AND USES: Metformin is a preferred oral antidiabetic drug for managing type 2 DM because of its effectiveness and safety. It is u...
-
INTRODUCTION: There are two sites of exchange of oxygen and carbon dioxide: the lungs and the tissues of the body. The exchange of gases ...
-
INTRODUCTION: Streptomycin was isolated from a strain of Streptomyces griseus. The antimicrobial activity of streptomycin is typical of ...
-
WINDOWS 10 INBUILT TOOLS: Windows 10 came inbuilt with many features that are not direct for a basic use, but when they are very useful. ...
-
Introduction: This is the amount of drug that reaches systemic circulation following administration using any of the drug administration r...
-
I MMUNOGLOBULIN G (IgG) : IgG contains two heavy chains and two light chains; heavy chains being of gamma type. Due to its sedimentation c...
-
ASSESSMENT AND CLASSIFICATION OF PAIN: The psychological reaction to pain is subjective. During physical assessment, the same degree and ty...
-
UGANDAN GOSPEL MUSIC JUDITH BABIRYE 1. Butonotono Download mp3 2. Nzijukira Download mp3 3. Judith Babirye non-stop music 2015 Download M...














.jpg)