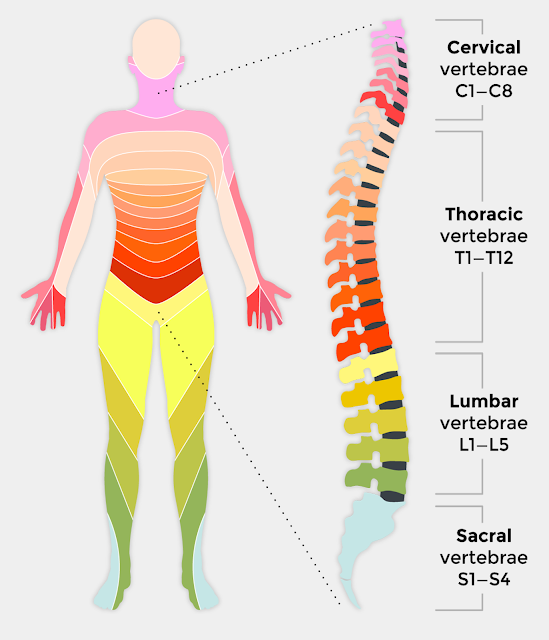
INTRODUCTION: Spinal cord injuries (SCIs) are a major health problem. Most SCIs result from motor vehicle crashes. Other causes include falls, violence especially primarily from gunshot wounds, and recreational sporting activities. Half of the victims are between 16 and 30 years of age; most are males. Another risk factor is substance abuse (alcohol and drugs). There is a high frequency of associated injuries and medical complications. The vertebrae most frequently involved in SCIs are the fifth, sixth, and seventh cervical vertebrae (C5–C7), the 12th thoracic vertebra (T12), and the first lumbar vertebra (L1). These vertebrae are the most susceptible because there is a greater range of mobility in the vertebral column in these areas.
Damage to the spinal cord ranges from transient concussion (patient recovers fully), to contusion, laceration, and compression of the cord substance (either alone or in combination), to complete transection of the cord (paralysis below the level of injury). Injury can be categorized as primary (usually permanent) or secondary (nerve fibers swell and disintegrate as a result of ischemia, hypoxia, edema, and hemorrhagic lesions). Whereas a primary injury is permanent, a secondary injury may be reversible if treated within 4 to 6 hours of the initial injury. The type of injury refers to the extent of injury to the spinal cord itself. Incomplete spinal cord lesions are classified according to the area of spinal cord damage: central, lateral, anterior, or peripheral. A complete SCI can result in paraplegia (paralysis of the lower body) or tetraplegia (formerly quadriplegia— paralysis of all four extremities).
CLINICAL MANIFESTATIONS: The consequences of SCI depend on the type and level of injury of the cord.
Neurologic Level: The neurologic level refers to the lowest level at which sensory and motor functions are normal. Signs and symptoms include the following: Total sensory and motor paralysis below the neurologic level. Loss of bladder and bowel control (usually with urinary retention and bladder distention). Loss of sweating and vasomotor tone. Marked reduction of BP from loss of peripheral vascular resistance. If conscious, patient reports acute pain in back or neck; patient may speak of fear that the neck or back is broken.
Respiratory Problems: Related to compromised respiratory function; severity depends on level of injury. Acute respiratory failure is the leading cause of death in high cervical cord injury.
ASSESSMENT AND DIAGNOSTIC METHODS: Detailed neurologic examination, x-ray examinations (lateral cervical spine x-rays), computed tomography (CT), magnetic resonance imaging (MRI), and ECG (bradycardia and asystole are common in acute spinal injuries) are common assessment and diagnostic methods.
COMPLICATIONS: Spinal shock, a serious complication of SCI, is a sudden depression of reflex activity in the spinal cord (areflexia) below the level of injury. The muscles innervated by the part of the cord segment situated below the level of the lesion become completely paralyzed and flaccid, and the reflexes are absent. BP and heart rate fall as vital organs are affected. Parts of the body below the level of the cord lesion are paralyzed and without sensation.
EMERGENCY MANAGEMENT: Immediate patient management at the accident scene is crucial. Improper handling can cause further damage and loss of neurologic function. Consider any victim of a motor vehicle crash, a diving or contact sports injury, a fall, or any direct trauma to the head and neck as having an SCI until ruled out. Initial care includes rapid assessment, immobilization, extrication, stabilization or control of life-threatening injuries, and transportation to an appropriate medical facility. Maintain patient in an extended position (not sitting); no body part should be twisted or turned. The standard of care is referral to a regional spinal injury center or trauma center for treatment in first 24 hours.
MEDICAL MANAGEMENT: Acute Phase Goals of management are to prevent further SCI and to observe for symptoms of progressive neurologic deficits. The patient is resuscitated as necessary, and oxygenation and cardiovascular stability are maintained. High-dose corticosteroids (methylprednisolone) may be administered to counteract spinal cord edema. Oxygen is administered to maintain a high arterial PaO2. Extreme care is taken to avoid flexing or extending the neck if endotracheal intubation is necessary. Diaphragm pacing (electrical stimulation of the phrenic nerve) may be considered for patients with high cervical spine injuries. SCI requires immobilization, reduction of dislocations, and stabilization of the vertebral column. The cervical fracture is reduced and the cervical spine aligned with a form of skeletal traction (using skeletal tongs or calipers or the halo-vest technique). Weights are hung freely so as not to interfere with the traction. Early surgery reduces the need for traction. The goals of surgical treatment are to preserve neurologic function by removing pressure from the spinal cord and to provide stability.
MANAGEMENT OF COMPLICATIONS:
Spinal and Neurogenic Shock: Intestinal decompression is used to treat bowel distention and paralytic ileus caused by depression of reflexes. This loss of sympathetic innervation causes a variety of other clinical manifestations, including neurogenic shock signaled by decreased cardiac output, venous pooling in the extremities, and peripheral vasodilation. Patient who does not perspire on paralyzed portion of body requires close observation for early detection of an abrupt onset of fever. Body defenses are maintained and supported until the spinal shock abates and the system has recovered from the traumatic insult (up to 4 months).
RELATED;
3. ACTIVATION OF A NERVE IMPULSE
4. BACK PAIN











No comments:
Post a Comment